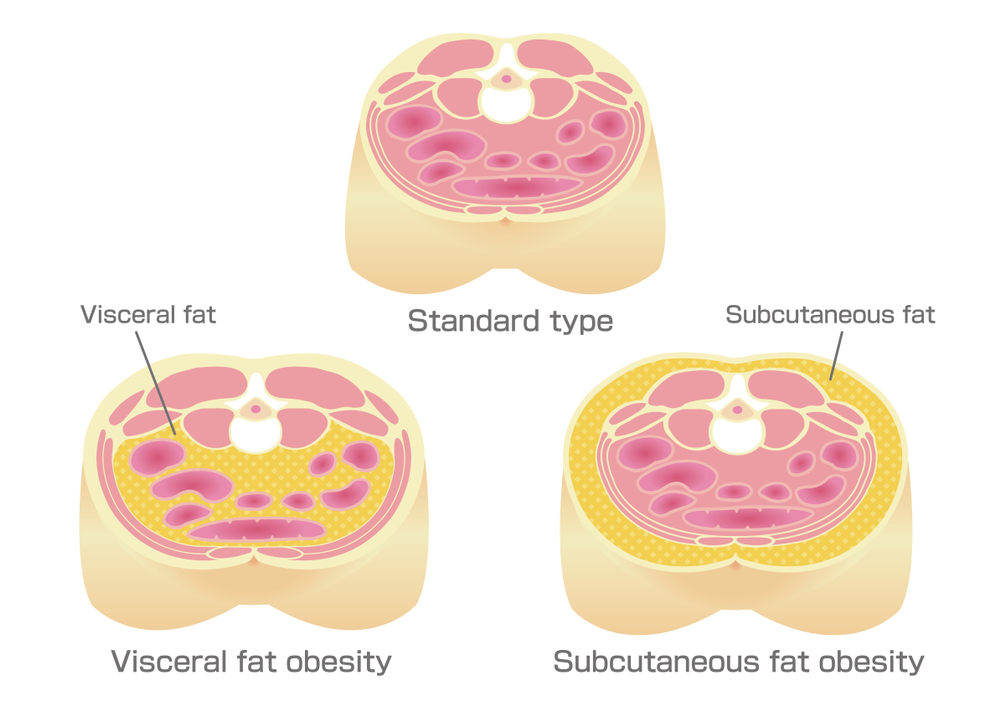
This has always been a topic of debate whether it’s the high BMI that needs to be considered as a risk factor for Insulin Resistance (IR) and Type 2 Diabetes Mellitus (DM) or the distribution of fat in the body matters. The objective of this article is to get into the details of the overall impact of BMI on IR and the difference between the subcutaneous fat and visceral fat that impacts the IR and thus leads to type 2 DM.
This has been proven by multiple studies in the past that high BMI corresponds to high-risk factors for lifestyle disorders but looking at BMI only will be a unidimensional approach as it doesn’t take into consideration the waist-hip ratio, body fat percentage, and distribution of fat in the body (subcutaneous fat Vs visceral fat)
As per the study done by Stefan et al many individuals, especially women despite having high BMI (as high as 50 to 60kg/m 2 ) remain insulin sensitive and normoglycemic, and the reason is high levels of subcutaneous fat in these individuals instead of visceral or ectopic fat. Also, a study done by McLaughlin et al in 2011 had concluded that after adjusting for BMI, greater absolute or relative Visceral Adipose Tissue increases the risk of IR whereas an increase in Subcutaneous Adipose Tissue has the opposite effect.
The increase in visceral fat or ectopic fat is attributed to a mechanism called Lipotoxicity which means deleterious effects of lipid accumulation in non-adipose tissues. Whenever there are an excessive amount of lipids in the body, the subcutaneous fat stores get overwhelmed which leads to the failure of accumulation of excess lipids into lipid droplets, causing chronic elevation of circulatory fatty acids and thus reaching toxic levels in non-adipose tissues.
Also, there is a marked difference between the characteristics of subcutaneous fat and visceral fat and as per the research done by Matsuzawa et al. In 1995, visceral fat was metabolically very active and released free fatty acids into the portal circulation, which enters into the liver directly. This leads to an increase in lipid biosynthesis in the liver and can cause IR resulting in hyperlipidemia, DM, and hypertension .
A study done by Mary Ann Banerji et al on Asian Indian Men in 1999 has also studied the degree of IR in the subjects having a normal BMI of 24.5 kg/m 2. CT measurements of these individuals showed their BF% in the range of 33 ± 7% which falls into the obese category. Almost 81% of this fat was distributed to the subcutaneous region whereas 16.8% was located in the intra abdominal or visceral component. Once they correlated the insulin action with adiposity, visceral adipose tissue was significantly related to insulin-mediated glucose disposal whereas total, as well as subcutaneous fat deposits, were non significant here. This study also inferred the direct relationship between IR and Visceral fat tissue.
So, to conclude from all the studies we have seen so far, more than BMI, it is the accumulation of fat and specifically the visceral fat which is responsible for increased IR in an individual and increases the risk for type 2 DM. Also, a study done by Fujioka et al in 1991 has shown that reduction in weight by calorie deficit diet resulting in a reduction of visceral fat volume and an overall reduction in visceral/subcutaneous fat ratio improves plasma glucose and lipid metabolism compared to decrease in body weight alone.
Reference list
- Banerji, M.A., Faridi, N., Atluri, R., Chaiken, R.L. and Lebovitz, H.E. (1999). Body Composition, Visceral Fat, Leptin, and Insulin Resistance in Asian Indian Men1. The Journal of Clinical Endocrinology & Metabolism, 84(1), pp.137–144.
- Engin, A.B. (2017). What Is Lipotoxicity? Advances in Experimental Medicine and Biology, [online] 960, pp.197–220.
- Fujioka, S., Matsuzawa, Y., Tokunaga, K., Kawamoto, T., Kobatake, T., Keno, Y., Kotani, K., Yoshida, S. and Tarui, S. (1991). Improvement of glucose and lipid metabolism associated with selective reduction of intra-abdominal visceral fat in premenopausal women with visceral fat obesity. International Journal of Obesity, [online] 15(12), pp.853–859. Available at: https://pubmed.ncbi.nlm.nih.gov/1794928/ [Accessed 11 Feb. 2022].
- Matsuzawa, Y., Shimomura, I., Nakamura, T., Keno, Y., Kotani, K. and Tokunaga, K. (1995). Pathophysiology and pathogenesis of visceral fat obesity. Obesity Research, [online] 3 Suppl 2, pp.187S194S.
- McLaughlin, T., Lamendola, C., Liu, A. and Abbasi, F. (2011). Preferential Fat Deposition in SubcutaneousVersusVisceral Depots Is Associated with Insulin Sensitivity. The Journal of Clinical Endocrinology & Metabolism, 96(11), pp.E1756–E1760.
- Stefan, N. (2008). Identification and Characterization of Metabolically Benign Obesity in Humans. Archives of Internal Medicine, 168(15), p.1609.